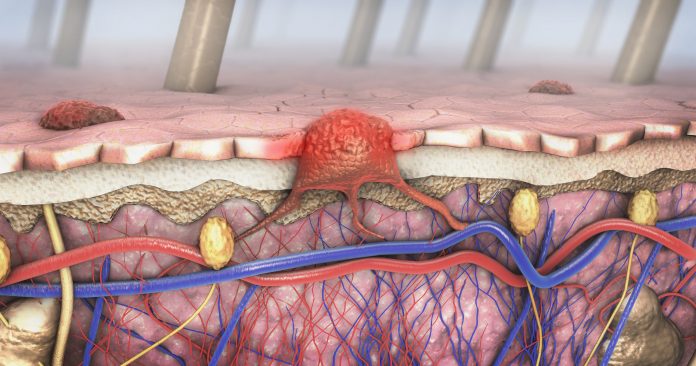
Metastases from primary cancer tumors may remain dormant in distant tissues for many years or decades before they re-emerge and grow new tumors. While many factors influence this process, one remains unquestioned: individuals with the tumors grow older. A new mice study published in Nature from investigators from Johns Hopkins makes a connection between melanoma cancer re-emergence and age-related influences.
The team asked two primary questions: do melanoma tumor cells travel to the organs of old and young mice at the same rate? Do they stay as single cell colonies in the young but then start to grow into new tumors as the animals age?
The study found that when melanoma cells were injected into the skin of young (8 weeks old, equivalent to young adult human) and older mice (18 months old, equivalent to humans aged 55 to 65), they traveled to the lungs at similar rates initially. But they grew much more slowly in the aged skin microenvironment, specifically in fibroblast stromal cells. “As the mice age they secrete certain factors that make these cancer cells grow very slowly, but it allows them to move much more efficiently,” explained first author Mitchell Fane, PhD. This causes these cancer cells to move away from the tumor and go into the bloodstream where they can circulate into the lung.
“But the difference we found is that once the melanoma cells got to the aged lung, they were actually not growing slowly, but they were growing really rapidly and formed larger tumors,” said Fane. In the younger lung, they tended to remain as small, single-cell or double-cell colonies.
Diving deeper into analyzing fibroblasts in the aged lung, they discovered that these fibroblasts secreted very different factors unlike those in aged skin. “These factors were causing the melanoma cells to grow much more rapidly in the lung,” added Fine, who discovered that a factor called secreted frizzled related protein 1 (SFRP1) inhibited the WNT5 signaling pathway which has a known role in melanoma metastasis. These factors secreted by aged lung fibroblasts inhibited WNT5, specifically WNT5A, and consequently allowed the melanoma cells to grow quickly. In contrast, young lung fibroblasts did not secrete these factors and the cells remained in a state of dormancy unable to grow.
“These changes were very consistent with a phenomenon in melanoma we call phenotype switching, in which melanoma exists either in a state of growing or invading,” noted senior author Ashani Weeraratna, PhD, co-leader of the cancer invasion and metastasis program at the Johns Hopkins Kimmel Cancer Center. “What our data showed is that these cells use different arms of the WNT pathway to switch back and forth between these two states. When the WNT5A signaling pathway is activated, the cells are highly invasive but not very proliferative and don’t grow fast. By contrast, when the WNT5A signaling pathway is suppressed, the cells grow much faster.”
The team has since found other factors—such as changes in the biophysical structure of the lung and the immune microenvironment—contribute to the process of re-emergence so indicating re-emergence is much more complex than just targeting the signaling pathways.
But Weeraratna cautions targeting WNT5 exclusively as a potential therapeutic approach. “We need to be more creative about these strategies as we don’t want to cause the cells to break from the primary tumor immediately,” she says. “We’re going to target the cells ultimately, but maybe it’s the microenvironment we want to be targeting rather than the cells themselves.” The team hopes this work may ultimately lead to improving the efficiency and outcomes of immunotherapy in melanoma.













